


AIDS was first reported June 5, 1981, when the U.S. Centers for Disease Control (CDC) recorded a cluster ofPneumocystis cariniipneumonia(now still classified as PCP but known to be caused byPneumocystis jirovecii) in five homosexual men in Los Angeles. In the beginning, the CDC did not have an official name for the disease, often referring to it by way of the diseases that were associated with it, for example,lymphadenopathy, the disease after which the discoverers of HIV originally named the virus. They also used Kaposi's Sarcoma and Opportunistic Infections, the name by which a task force had been set up in 1981.

In the general press, the termGRID, which stood for Gay-related immune deficiency, had been coined. The CDC, in search of a name, and looking at the infected communities coined “the 4H disease,” as it seemed to single out Haitians, homosexuals, hemophiliacs, and heroinusers. However, after determining that AIDS was not isolated to the homosexual community, the term GRID became misleading andAIDS was introduced at a meeting in July 1982. By September 1982 the CDC started using the name AIDS, and properly defined the illness.
A more controversial theory known as the OPV AIDS hypothesis suggests that the AIDS epidemic was inadvertently started in the late 1950s in the Belgian Congo by Hilary Koprowski's research into a poliomyelitis vaccine. According to scientific consensus, this scenario is not supported by the available evidence.
A recent study states that HIV probably moved from Africa to Haiti and then entered the United States around 1969.

The symptoms of AIDS are primarily the result of conditions that do not normally develop in individuals with healthy immune systems. Most of these conditions are infections caused bybacteria, viruses, fungi and parasites that are normally controlled by the elements of the immune system that HIV damages. 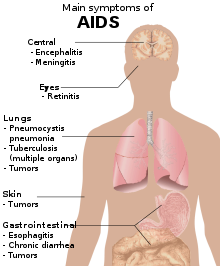
Opportunistic infections are common in people with AIDS.These infections affect nearly everyorgan system.
People with AIDS also have an increased risk of developing various cancers such as Kaposi's sarcoma, cervical cancer and cancers of the immune system known as lymphomas. Additionally, people with AIDS often have systemic symptoms of infection like fevers, sweats (particularly at night), swollen glands, chills, weakness, and weight loss. The specific opportunistic infections that AIDS patients develop depend in part on the prevalence of these infections in the geographic area in which the patient lives.
 [HIV patient]
[HIV patient]
Pulmonary infections :
Pneumocystis pneumonia (originally known asPneumocystis cariniipneumonia, and still abbreviated as PCP, which now stands for Pneumocystis pneumonia) is relatively rare in healthy,immunocompetent people, but common among HIV-infected individuals. It is caused byPneumocystis jirovecii.
Before the advent of effective diagnosis, treatment and routine prophylaxis in Western countries, it was a common immediate cause of death. In developing countries, it is still one of the first indications of AIDS in untested individuals, although it does not generally occur unless the CD4 count is less than 200 cells per µL of blood.
Tuberculosis (TB) is unique among infections associated with HIV because it is transmissible to immunocompetent people via the respiratory route, is not easily treatable once identified, may occur in early-stage HIV disease, and is preventable with drug therapy. However,multidrug resistance is a serious problem. Tuberculosis with HIV co-infection (TB/HIV) is a major world health problem according to the World Health Organization: in 2007, 456,000 deaths among incident TB cases were HIV-positive, a third of all TB deaths and nearly a quarter of the estimated 2 million HIV deaths in that year.
Even though its incidence has declined because of the use of directly observed therapy and other improved practices in Western countries, this is not the case in developing countries where HIV is most prevalent. In early-stage HIV infection (CD4 count >300 cells per µL), TB typically presents as a pulmonary disease. In advanced HIV infection, TB often presents atypically with extrapulmonary (systemic) disease a common feature. Symptoms are usually constitutional and are not localized to one particular site, often affecting bone marrow, bone, urinary and gastrointestinal tracts, liver, regional lymph nodes, and the central nervous system.
Gastrointestinal infections :
Esophagitis is an inflammation of the lining of the lower end of the esophagus (gullet or swallowing tube leading to the stomach). In HIV infected individuals, this is normally due to fungal (candidiasis) or viral (herpes simplex-1 or cytomegalovirus) infections. In rare cases, it could be due tomycobacteria.
Unexplained chronic diarrhea in HIV infection is due to many possible causes, including common bacterial (Salmonella, Shigella, Listeriaor Campylobacter) and parasitic infections; and uncommon opportunistic infections such as cryptosporidiosis, microsporidiosis,Mycobacterium aviumcomplex (MAC) and viruses,astrovirus, adenovirus, rotavirus and cytomegalovirus, (the latter as a course of colitis).
In some cases, diarrhea may be a side effect of several drugs used to treat HIV, or it may simply accompany HIV infection, particularly during primary HIV infection. It may also be a side effect ofantibiotics used to treat bacterial causes of diarrhea (common forClostridium difficile). In the later stages of HIV infection, diarrhea is thought to be a reflection of changes in the way the intestinal tract absorbs nutrients, and may be an important component of HIV-related wasting.
Neurological and psychiatric involvement :
HIV infection may lead to a variety of neuropsychiatric sequelae, either by infection of the now susceptible nervous system by organisms, or as a direct consequence of the illness itself.

Toxoplasmosis is a disease caused by the single-celled parasite called Toxoplasma gondii; it usually infects the brain, causing toxoplasmaencephalitis, but it can also infect and cause disease in the eyes and lungs. Cryptococcal meningitis is an infection of the meninx (the membrane covering the brain and spinal cord) by the fungusCryptococcus neoformans. It can cause fevers, headache, fatigue, nausea, andvomiting. Patients may also develop seizures and confusion; left untreated, it can be lethal.
Progressive multifocal leukoencephalopathy (PML) is a demyelinating disease, in which the gradual destruction of the myelin sheath covering the axons of nerve cells impairs the transmission of nerve impulses. It is caused by a virus called JC virus which occurs in 70% of the population in latent form, causing disease only when the immune system has been severely weakened, as is the case for AIDS patients. It progresses rapidly, usually causing death within months of diagnosis.
AIDS dementia complex (ADC) is a metabolic encephalopathy induced by HIV infection and fueled by immune activation of HIV infected brainmacrophages and microglia. These cells are productively infected by HIV and secrete neurotoxins of both host and viral origin.Specific neurological impairments are manifested by cognitive, behavioral, and motor abnormalities that occur after years of HIV infection and are associated with low CD4+ T cell levels and high plasma viral loads.
Prevalence is 10–20% in Western countries but only 1–2% of HIV infections in India. This difference is possibly due to the HIV subtype in India. AIDS related mania is sometimes seen in patients with advanced HIV illness; it presents with more irritability and cognitive impairment and less euphoria than a manic episode associated with true bipolar disorder. Unlike the latter condition, it may have a more chronic course. This syndrome is less often seen with the advent of multi-drug therapy.
Tumors and malignancies :
Patients with HIV infection have substantially increased incidence of several cancers. This is primarily due to co-infection with an oncogenic DNA virus, especially Epstein-Barr virus (EBV),Kaposi's sarcoma-associated herpesvirus (KSHV) (also known as human herpesvirus-8 [HHV-8]), and human papillomavirus (HPV).
Kaposi's sarcoma (KS) is the most common tumor in HIV-infected patients. The appearance of this tumor in young homosexual men in 1981 was one of the first signals of the AIDS epidemic. Caused by a gammaherpes virus called Kaposi's sarcoma-associated herpes virus (KSHV), it often appears as purplish nodules on the skin, but can affect other organs, especially the mouth, gastrointestinal tract, and lungs. High-grade B cell lymphomas such as Burkitt's lymphoma, Burkitt's-like lymphoma, diffuse large B-cell lymphoma (DLBCL), and primary central nervous system lymphoma present more often in HIV-infected patients. These particular cancers often foreshadow a poor prognosis. Epstein-Barr virus (EBV) or KSHV cause many of these lymphomas. In HIV-infected patients, lymphoma often arises in extranodal sites such as the gastrointestinal tract. When they occur in an HIV-infected patient, KS and aggressive B cell lymphomas confer a diagnosis of AIDS.
Invasive cervical cancer in HIV-infected women is also considered AIDS-defining. It is caused by human papillomavirus (HPV).
In addition to the AIDS-defining tumors listed above, HIV-infected patients are at increased risk of certain other tumors, notably Hodgkin's disease, anal and rectal carcinomas, hepatocellular carcinomas, head and neck cancers, and lung cancer. Some of these are causes by viruses, such as Hodgkin's disease (EBV), anal/rectal cancers (HPV), head and neck cancers (HPV), and hepatocellular carcinoma (hepatitis B or C). Other contributing factors include exposure to carcinogens (cigarette smoke for lung cancer), or living for years with subtle immune defects.
Interestingly, the incidence of many common tumors, such as breast cancer or colon cancer, does not increase in HIV-infected patients. In areas where HAART is extensively used to treat AIDS, the incidence of many AIDS-related malignancies has decreased, but at the same time malignant cancers overall have become the most common cause of death of HIV-infected patients. In recent years, an increasing proportion of these deaths have been from non-AIDS-defining cancers.
Other infections :
AIDS patients often develop opportunistic infections that present with non-specific symptoms, especially low-grade fevers and weight loss. These include opportunistic infection with Mycobacterium avium-intracellulare and cytomegalovirus (CMV). CMV can cause colitis, as described above, and CMV retinitis can cause blindness.
Penicilliosis due toPenicillium marneffei is now the third most common opportunistic infection (after extrapulmonary tuberculosis andcryptococcosis) in HIV-positive individuals within the endemic area of Southeast Asia.
An infection that often goes unrecognized in AIDS patients is Parvovirus B19. Its main consequence is anemia, which is difficult to distinguish from the effects of antiretroviral drugs used to treat AIDS itself.
CAUSE :
AIDS is the most severe acceleration of infection with HIV. HIV is a retrovirus that primarily infects vital organs of the human immune system such as CD4+ T cells (a subset of T cells), macrophagesand dendritic cells. It directly and indirectly destroys CD4+ T cells.
Once HIV has killed so many CD4+ T cells that there are fewer than 200 of these cells per microliter(µL) of blood, cellular immunity is lost. Acute HIV infection progresses over time to clinical latent HIV infection and then to early symptomatic HIV infection and later to AIDS, which is identified either on the basis of the amount of CD4+ T cells remaining in the blood, and/or the presence of certain infections, as noted above.
In the absence of antiretroviral therapy, the median time of progression from HIV infection to AIDS is nine to ten years, and the median survival time after developing AIDS is only 9.2 months. However, the rate of clinical disease progression varies widely between individuals, from two weeks up to 20 years.
Many factors affect the rate of progression. These include factors that influence the body's ability to defend against HIV such as the infected person's general immune function. Older people have weaker immune systems, and therefore have a greater risk of rapid disease progression than younger people.
Poor access to health care and the existence of coexisting infections such as tuberculosis also may predispose people to faster disease progression. The infected person's genetic inheritance plays an important role and some people are resistant to certain strains of HIV. An example of this is people with the homozygous CCR5-Δ32 variation are resistant to infection with certain strains of HIV. HIV is genetically variable and exists as different strains, which cause different rates of clinical disease progression.
Sexual transmission :
Sexual transmission occurs with the contact between sexual secretions of one person with the rectal, genital or oral mucous membranes of another. Unprotected sexual acts are riskier for the receptive partner than for the insertive partner, and the risk for transmitting HIV through unprotected anal intercourse is greater than the risk from vaginal intercourse or oral sex.

However, oral sex is not entirely safe, as HIV can be transmitted through both insertive and receptive oral sex. Sexual assault greatly increases the risk of HIV transmission as condoms are rarely employed and physical trauma to the vagina or rectum occurs frequently, facilitating the transmission of HIV.
Other sexually transmitted infections (STI) increase the risk of HIV transmission and infection, because they cause the disruption of the normalepithelial barrier by genital ulceration and/or microulceration; and by accumulation of pools of HIV-susceptible or HIV-infected cells (lymphocytes and macrophages) in semen and vaginal secretions. Epidemiological studies from sub-Saharan Africa, Europe and North Americasuggest that genital ulcers, such as those caused by syphilis and/or chancroid, increase the risk of becoming infected with HIV by about fourfold. There is also a significant although lesser increase in risk from STIs such as gonorrhea, chlamydia and trichomoniasis, which all cause local accumulations of lymphocytes and macrophages.
Transmission of HIV depends on the infectiousness of the index case and the susceptibility of the uninfected partner. Infectivity seems to vary during the course of illness and is not constant between individuals. An undetectable plasma viral load does not necessarily indicate a low viral load in the seminal liquid or genital secretions.
However, each 10-fold increase in the level of HIV in the blood is associated with an 81% increased rate of HIV transmission. Women are more susceptible to HIV-1 infection due to hormonal changes, vaginal microbial ecology and physiology, and a higher prevalence of sexually transmitted diseases.
People who have been infected with one strain of HIV can still be infected later on in their lives by other, more virulent strains.

Infection is unlikely in a single encounter. High rates of infection have been linked to a pattern of overlapping long-term sexual relationships. This allows the virus to quickly spread to multiple partners who in turn infect their partners. A pattern of serial monogamy or occasional casual encounters is associated with lower rates of infection.
HIV spreads readily through heterosexual sex in Africa, but less so elsewhere. One possibility being researched is that schistosomiasis, which affects up to 50% of women in parts of Africa, damages the lining of the vagina.
Exposure to blood-borne pathogens :
This transmission route is particularly relevant to intravenous drug users, hemophiliacs and recipients of blood transfusions and blood products. Sharing and reusing syringes contaminated with HIV-infected blood represents a major risk for infection with HIV.
Needle sharing is the cause of one third of all new HIV-infections in North America, China, andEastern Europe. The risk of being infected with HIV from a single prick with a needle that has been used on an HIV-infected person is thought to be about 1 in 150 (see table above). Post-exposure prophylaxis with anti-HIV drugs can further reduce this risk.
This route can also affect people who give and receive tattoos and piercings. Universal precautionsare frequently not followed in both sub-Saharan Africa and much of Asia because of both a shortage of supplies and inadequate training.
The WHO estimates that approximately 2.5% of all HIV infections in sub-Saharan Africa are transmitted through unsafe healthcare injections. Because of this, the United Nations General Assembly has urged the nations of the world to implement precautions to prevent HIV transmission by health workers.
The risk of transmitting HIV to blood transfusion recipients is extremely low in developed countries where improved donor selection and HIV screening is performed. However, according to the WHO, the overwhelming majority of the world's population does not have access to safe blood and between 5% and 10% of the world's HIV infections come from transfusion of infected blood and blood products.
Perinatal transmission :
The transmission of the virus from the mother to the child can occur in utero during the last weeks of pregnancy and at childbirth. In the absence of treatment, the transmission rate between a mother and her child during pregnancy, labor and delivery is 25%.
However, when the mother takes antiretroviral therapy and gives birth by caesarean section, the rate of transmission is just 1%. The risk of infection is influenced by the viral load of the mother at birth, with the higher the viral load, the higher the risk. Breastfeeding also increases the risk of transmission by about 4 %.

Misconceptions :
A number of misconceptions have arisen surrounding HIV/AIDS. Three of the most common are that AIDS can spread through casual contact, that sexual intercourse with a virgin will cure AIDS, and that HIV can infect only homosexual men and drug users. Other misconceptions are that any act of anal intercourse between gay men can lead to AIDS infection, and that open
PATHOPHYSIOLOGY :
The pathophysiology of AIDS is complex, as is the case with all syndromes.Ultimately, HIV causes AIDS by depleting CD4+ T helper lymphocytes. This weakens the immune system and allows opportunistic infections. T lymphocytes are essential to the immune response and without them, the body cannot fight infections or kill cancerous cells. The mechanism of CD4+ T cell depletion differs in the acute and chronic phases.

During the acute phase, HIV-induced cell lysis and killing of infected cells by cytotoxic T cells accounts for CD4+ T cell depletion, althoughapoptosis may also be a factor. During the chronic phase, the consequences of generalized immune activation coupled with the gradual loss of the ability of the immune system to generate new T cells appear to account for the slow decline in CD4+ T cell numbers.
Although the symptoms of immune deficiency characteristic of AIDS do not appear for years after a person is infected, the bulk of CD4+ T cell loss occurs during the first weeks of infection, especially in the intestinal mucosa, which harbors the majority of the lymphocytes found in the body. The reason for the preferential loss of mucosal CD4+T cells is that a majority of mucosal CD4+ T cells express the CCR5 coreceptor, whereas a small fraction of CD4+ T cells in the bloodstream do so.
HIV seeks out and destroys CCR5 expressing CD4+ cells during acute infection. A vigorous immune response eventually controls the infection and initiates the clinically latent phase. However, CD4+ T cells in mucosal tissues remain depleted throughout the infection, although enough remain to initially ward off life-threatening infections.
Continuous HIV replication results in a state of generalized immune activation persisting throughout the chronic phase. Immune activation, which is reflected by the increased activation state of immune cells and release of proinflammatory cytokines, results from the activity of several HIV gene products and the immune response to ongoing HIV replication. Another cause is the breakdown of the immune surveillance system of the mucosal barrier caused by the depletion of mucosal CD4+ T cells during the acute phase of disease.
This results in the systemic exposure of the immune system to microbial components of the gut’s normal flora, which in a healthy person is kept in check by the mucosal immune system. The activation and proliferation of T cells that results from immune activation provides fresh targets for HIV infection. However, direct killing by HIV alone cannot account for the observed depletion of CD4+ T cells since only 0.01–0.10% of CD4+ T cells in the blood are infected.
A major cause of CD4+ T cell loss appears to result from their heightened susceptibility to apoptosis when the immune system remains activated. Although new T cells are continuously produced by the thymus to replace the ones lost, the regenerative capacity of the thymus is slowly destroyed by direct infection of its thymocytes by HIV. Eventually, the minimal number of CD4+ T cells necessary to maintain a sufficient immune response is lost, leading to AIDS.
Cells affected :
The virus, entering through which ever route, acts primarily on the following cells:
- Lymphoreticular system:
- CD4+ T-Helper cells
- Macrophages
- Monocytes
- B-lymphocytes
- Certain endothelial cells
- Central nervous system:
- Microglia of the nervous system
- Astrocytes
- Oligodendrocytes
- Neurones – indirectly by the action of cytokines and the gp-120
The effect
The virus has cytopathic effects but how it does it is still not quite clear. It can remain inactive in these cells for long periods, though. This effect is hypothesized to be due to the CD4-gp120 interaction.
- The most prominent effect of HIV is its T-helper cell suppression and lysis. The cell is simply killed off or deranged to the point of being function-less (they do not respond to foreign antigens). The infected B-cells can not produce enough antibodies either. Thus the immune system collapses leading to the familiar AIDS complications, like infections and neoplasms (vide supra).
- Infection of the cells of the CNS cause acute aseptic meningitis, subacute encephalitis, vacuolar myelopathy and peripheral neuropathy. Later it leads to even AIDS dementia complex.
- The CD4-gp120 interaction (see above) is also permissive to other viruses like Cytomegalovirus, Hepatitis virus, Herpes simplex virus, etc. These viruses lead to further cell damage i.e. cytopathy.
DIAGNOSIS :
The diagnosis of AIDS in a person infected with HIV is based on the presence of certain signs or symptoms. Since June 5, 1981, many definitions have been developed for epidemiological surveillance such as the Bangui definition and the 1994 expanded World Health Organization AIDS case definition. However, clinical staging of patients was not an intended use for these systems as they are neither sensitive, nor specific. In developing countries, the World Health Organization staging system for HIV infection and disease, using clinical and laboratory data, is used and in developed countries, the Centers for Disease Control (CDC) Classification System is used.
WHO disease staging system :
In 1990, the World Health Organization (WHO) grouped these infections and conditions together by introducing a staging system for patients infected with HIV-1. An update took place in September 2005. Most of these conditions are opportunistic infections that are easily treatable in healthy people.
- Stage I: HIV infection is asymptomatic and not categorized as AIDS
- Stage II: includes minor mucocutaneous manifestations and recurrent upper respiratory tract infections
- Stage III: includes unexplained chronic diarrhea for longer than a month, severe bacterial infections and pulmonary tuberculosis
- Stage IV: includes toxoplasmosis of the brain, candidiasis of the esophagus, trachea, bronchi or lungs and Kaposi's sarcoma; these diseases are indicators of AIDS.
CDC classification system :
There are two main definitions for AIDS, both produced by the Centers for Disease Control and Prevention (CDC). The older definition is to referring to AIDS using the diseases that were associated with it, for example, lymphadenopathy, the disease after which the discoverers of HIV originally named the virus.In 1993, the CDC expanded their definition of AIDS to include all HIV positive people with a CD4+ T cell count below 200 per µL of blood or 14% of all lymphocytes. The majority of new AIDS cases in developed countries use either this definition or the pre-1993 CDC definition. The AIDS diagnosis still stands even if, after treatment, the CD4+ T cell count rises to above 200 per µL of blood or other AIDS-defining illnesses are cured.
HIV test :
Many people are unaware that they are infected with HIV. Less than 1% of the sexually active urban population in Africa has been tested, and this proportion is even lower in rural populations. Furthermore, only 0.5% of pregnant women attending urban health facilities are counseled, tested or receive their test results. Again, this proportion is even lower in rural health facilities. Therefore, donor blood and blood products used in medicine and medical research are screened for HIV.
HIV tests are usually performed on venous blood. Many laboratories use fourth generationscreening tests which detect anti-HIV antibody (IgG and IgM) and the HIV p24 antigen. The detection of HIV antibody or antigen in a patient previously known to be negative is evidence of HIV infection. Individuals whose first specimen indicates evidence of HIV infection will have a repeat test on a second blood sample to confirm the results.
The window period (the time between initial infection and the development of detectable antibodies against the infection) can vary since it can take 3–6 months to seroconvert and to test positive. Detection of the virus using polymerase chain reaction (PCR) during the window period is possible, and evidence suggests that an infection may often be detected earlier than when using a fourth generation EIA screening test.
Positive results obtained by PCR are confirmed by antibody tests. Routinely used HIV tests for infection in neonates and infants (i.e., patients younger than 2 years), born to HIV-positive mothers, have no value because of the presence of maternal antibody to HIV in the child's blood. HIV infection can only be diagnosed by PCR, testing for HIV pro-viral DNA in the children's lymphocytes.
PREVENTION :
The three main transmission routes of HIV are sexual contact, exposure to infected body fluids or tissues, and from mother to fetus or child duringperinatal period. It is possible to find HIV in the saliva, tears, and urine of infected individuals, but there are no recorded cases of infection by these secretions, and the risk of infection is negligible.
Sexual contact :
The majority of HIV infections are acquired through unprotected sexualrelations between partners, one of whom has HIV. The primary mode of HIV infection worldwide is through sexual contact between members of the opposite sex.
During a sexual act, only male or female condoms can reduce the chances of infection with HIV and other STDs and the chances of becoming pregnant. The best evidence to date indicates that typical condom use reduces the risk ofheterosexual HIV transmission by approximately 80% over the long-term, though the benefit is likely to be higher if condoms are used correctly on every occasion.
The male latex condom, if used correctly without oil-based lubricants, is the single most effective available technology to reduce the sexual transmission of HIV and other sexually transmitted infections. Manufacturers recommend that oil-based lubricants such as petroleum jelly, butter, and lard not be used with latex condoms, because they dissolve the latex, making the condoms porous. If necessary, manufacturers recommend using water-based lubricants.
Oil-based lubricants can however be used with polyurethane condoms.
The female condom is an alternative to the male condom and is made from polyurethane, which allows it to be used in the presence of oil-based lubricants. They are larger than male condoms and have a stiffened ring-shaped opening, and are designed to be inserted into the vagina.
The female condom contains an inner ring, which keeps the condom in place inside the vagina – inserting the female condom requires squeezing this ring. However, at present availability of female condoms is very low and the price remains prohibitive for many women.
Preliminary studies suggest that, where female condoms are available, overall protected sexual acts increase relative to unprotected sexual acts, making them an important HIV prevention strategy.
Studies on couples where one partner is infected show that with consistent condom use, HIV infection rates for the uninfected partner are below 1% per year. Prevention strategies, like are well-known in developed countries, but epidemiological and behavioral studies in Europe and North America suggest that a substantial minority of young people continue to engage in high-risk practices despite HIV/AIDS knowledge, underestimating their own risk of becoming infected with HIV.
Randomized controlled trials have shown that male circumcision lowers the risk of HIV infection among heterosexual men by up to 60%. It is expected that this procedure will be actively promoted in many of the countries affected by HIV, although doing so will involve confronting a number of practical, cultural and attitudinal issues. However, programs to encourage condom use, including providing them free to those in poverty, are estimated to be 95 times more cost effective than circumcision at reducing the rate of HIV in sub-Saharan Africa.
Some experts fear that a lower perception of vulnerability among circumcised men may result in more sexual risk-taking behavior, thus negating its preventive effects. However, one randomized controlled trial indicated that adult male circumcision was not associated with increased HIV risk behavior.
Exposure to infected body fluids :
Health care workers can reduce exposure to HIV by employing precautions to reduce the risk of exposure to contaminated blood. These precautions include barriers such as gloves, masks, protective eyeware or shields, and gowns or aprons which prevent exposure of the skin or mucous membranes to blood borne pathogens. Frequent and thorough washing of the skin immediately after being contaminated with blood or other bodily fluids can reduce the chance of infection. Finally, sharp objects like needles, scalpels and glass, are carefully disposed of to prevent needlestick injuries with contaminated items. Since intravenous drug use is an important factor in HIV transmission in developed countries, harm reduction strategies such as needle-exchange programmes are used in attempts to reduce the infections caused by drug abuse.
Mother-to-child transmission (MTCT) :
Current recommendations state that when replacement feeding is acceptable, feasible, affordable, sustainable and safe, HIV-infected mothers should avoid breast-feeding their infant. However, if this is not the case, exclusive breast-feeding is recommended during the first months of life and discontinued as soon as possible. It should be noted that women may breastfeed other children who are not their own; see wetnurse.
Education, health literacy and cognitive ability :
The most important way to change risky behavior is health education. Several studies have shown the positive impact of education and health literacy on cautious sex behavior. Education itself does not work, only if it leads to higher health literacy and general cognitive ability. This ability is relevant to understand the relationship between own risky behavior and possible outcomes like HIV-transmission.
TREATMENT :
There is currently no publicly available vaccine for HIV or cure for HIV or AIDS. The only known methods of prevention are based on avoiding exposure to the virus or, failing that, an antiretroviral treatment directly after a highly significant exposure, called post-exposure prophylaxis(PEP). PEP has a very demanding four week schedule of dosage. It also has very unpleasant side effects including diarrhea, malaise,nausea and fatigue. 
Antiviral therapy :
Current treatment for HIV infection consists of highly active antiretroviral therapy, or HAART. This has been highly beneficial to many HIV-infected individuals since its introduction in 1996 when the protease inhibitor-based HAART initially became available. Current optimal HAART options consist of combinations (or "cocktails") consisting of at least three drugs belonging to at least two types, or "classes," of antiretroviral agents.
Typical regimens consist of two nucleoside analogue reverse transcriptase inhibitors (NARTIs or NRTIs) plus either a protease inhibitor or a non-nucleoside reverse transcriptase inhibitor (NNRTI). Because HIV disease progression in children is more rapid than in adults, and laboratory parameters are less predictive of risk for disease progression, particularly for young infants, treatment recommendations are more aggressive for children than for adults. In developed countries where HAART is available, doctors assess the viral load, rapidity in CD4 decline, and patient readiness while deciding when to recommend initiating treatment.
Standard goals of HAART include improvement in the patient’s quality of life, reduction in complications, and reduction of HIV viremia below the limit of detection, but it does not cure the patient of HIV nor does it prevent the return, once treatment is stopped, of high blood levels of HIV, often HAART resistant.Moreover, it would take more than the lifetime of an individual to be cleared of HIV infection using HAART.
Despite this, many HIV-infected individuals have experienced remarkable improvements in their general health and quality of life, which has led to the plummeting of HIV-associated morbidity and mortality. In the absence of HAART, progression from HIV infection to AIDS occurs at amedian of between nine to ten years and the median survival time after developing AIDS is only 9.2 months. HAART is thought to increase survival time by between 4 and 12 years.
For some patients, which can be more than fifty percent of patients, HAART achieves far less than optimal results, due to medication intolerance/side effects, prior ineffective antiretroviral therapy and infection with a drug-resistant strain of HIV. Non-adherence and non-persistence with therapy are the major reasons why some people do not benefit from HAART. The reasons for non-adherence and non-persistence are varied. Major psychosocial issues include poor access to medical care, inadequate social supports, psychiatric disease and drug abuse. HAART regimens can also be complex and thus hard to follow, with large numbers of pills taken frequently.
Side effects can also deter people from persisting with HAART, these include lipodystrophy, dyslipidaemia, diarrhoea, insulin resistance, an increase in cardiovascular risks and birth defects.Anti-retroviral drugs are expensive, and the majority of the world's infected individuals do not have access to medications and treatments for HIV and AIDS.
Experimental and proposed treatments :
It has been postulated that only a vaccine can halt the pandemic because a vaccine would possibly cost less, thus being affordable for developing countries, and would not require daily treatments. However, even after almost 30 years of research, HIV-1 remains a difficult target for a vaccine.
Research to improve current treatments includes decreasing side effects of current drugs, further simplifying drug regimens to improve adherence, and determining the best sequence of regimens to manage drug resistance. A number of studies have shown that measures to prevent opportunistic infections can be beneficial when treating patients with HIV infection or AIDS. Vaccination against hepatitis A and B is advised for patients who are not infected with these viruses and are at risk of becoming infected. Patients with substantial immunosuppression are also advised to receive prophylactic therapy for Pneumocystis jiroveci pneumonia (PCP), and many patients may benefit from prophylactic therapy for toxoplasmosis and Cryptococcus meningitis as well.
Researchers have discovered an abzyme that can destroy the protein gp120 CD4 binding site. This protein is common to all HIV variants as it is the attachment point for B lymphocytes and subsequent compromising of the immune system.
In Berlin, Germany, a 42-year-old leukemia patient infected with HIV for more than a decade was given an experimental transplant of bone marrow with cells that contained an unusual natural variant of the CCR5 cell-surface receptor. This CCR5-Δ32 variant has been shown to make some cells from people who are born with it resistant to infection with some strains of HIV. Almost two years after the transplant, and even after the patient reportedly stopped taking antiretroviral medications, HIV has not been detected in the patient's blood.
Alternative medicine :
In the US, approximately 60% of HIV patients use various forms of alternative medicine.Despite the widespread use of CAM by people living with HIV/AIDS, the effectiveness of these therapies has not been established. A 2005 Cochrane review of existing high-quality scientific evidence concluded: "There is insufficient evidence to support the use of herbal medicines in HIV-infected individuals and AIDS patients." Acupuncture has only been proposed for symptomatic relief, but not to treat or cure HIV or AIDS.
Morbidity and mortality among HIV-infected adults with adequate dietary nutritional intake is unaffected by multivitaminsupplementation.A large Tanzanian trial in immunologically and nutritionally compromised pregnant and lactating women showed a number of benefits to daily multivitamin supplementation for both mothers and children.Dietary intake of micronutrients at RDA levels by HIV-infected adults is recommended by the World Health Organization. There is some evidence that vitamin A supplementation in children reduces mortality and improves growth.Daily doses of selenium can suppress HIV viral burden with an associated improvement of the CD4 count. Selenium can be used as an adjunct therapy to standard antiviral treatments, but cannot itself reduce mortality and morbidity.

GENERALLY ASKED QUESTIONS :
Should I get an HIV Test?
The following are behaviors that increase your chances of getting HIV. If you answer yes to any of them, you should definitely get an HIV test. If you continue with any of these behaviors, you should be tested every year. Talk to a health care provider about an HIV testing schedule that is right for you.
- Have you injected drugs or steroids or shared equipment (such as needles, syringes, works) with others?
- Have you had unprotected vaginal, anal, or oral sex with men who have sex with men, multiple partners, or anonymous partners?
- Have you exchanged sex for drugs or money?
- Have you been diagnosed with or treated for hepatitis, tuberculosis (TB), or a sexually transmitted disease (STD), like syphilis?
- Have you had unprotected sex with someone who could answer yes to any of the above questions?
If you have had sex with someone whose history of sex partners and/or drug use is unknown to you or if you or your partner has had many sex partners, then you have more of a chance of being infected with HIV. Both you and your new partner should get tested for HIV, and learn the results, before having sex for the first time.
For women who plan to become pregnant, testing is even more important. If a woman is infected with HIV, medical care and certain drugs given during pregnancy can lower the chance of passing HIV to her baby. All women who are pregnant should be tested during each pregnancy.
How long after a possible exposure should I wait to get tested for HIV?
Most HIV tests are antibody tests that measure the antibodies your body makes against HIV. It can take some time for the immune system to produce enough antibodies for the antibody test to detect and this time period can vary from person to person. This time period is commonly referred to as the “window period”. Most people will develop detectable antibodies within 2 to 8 weeks (the average is 25 days). Even so, there is a chance that some individuals will take longer to develop detectable antibodies. Therefore, if the initial negative HIV test was conducted within the first 3 months after possible exposure, repeat testing should be considered >3 months after the exposure occurred to account for the possibility of a false-negative result. Ninety seven percent will develop antibodies in the first 3 months following the time of their infection. In very rare cases, it can take up to 6 months to develop antibodies to HIV.
Another type of test is an RNA test, which detects the HIV virus directly. The time between HIV infection and RNA detection is 9-11 days. These tests, which are more costly and used less often than antibody tests, are used in some parts of the United States.
For information on HIV testing, you can talk to your health care provider or you can find the location of the HIV testing site nearest to you by callingCDC-INFO 24 Hours/Day at1-800-CDC-INFO (232-4636), 1-888-232-6348 (TTY), in English, en Español. Both of these resources are confidential.
How do HIV tests work?
Once HIV enters the body, the immune system starts to produce antibodies – (chemicals that are part of the immune system that recognize invaders like bacteria and viruses and mobilize the body's attempt to fight infection). In the case of HIV, these antibodies cannot fight off the infection, but their presence is used to tell whether a person has HIV in his or her body. In other words, most HIV tests look for the HIV antibodies rather than looking for HIV itself. There are tests that look for HIV's genetic material directly, but these are not in widespread use.
The most common HIV tests use blood to detect HIV infection. Tests using saliva or urine are also available. Some tests take a few days for results, but rapid HIV tests can give results in about 20 minutes. All positive HIV tests must be followed up by another test to confirm the positive result. Results of this confirmatory test can take a few days to a few weeks.
If I test HIV negative, does that mean that my sex partner is HIV negative also?
No. Your HIV test result reveals only your HIV status. Your negative test result does not indicate whether or not your partner has HIV. HIV is not necessarily transmitted every time you have sex. Therefore, your taking an HIV test should not be seen as a method to find out if your partner is infected.
Ask your partner if he or she has been tested for HIV and what risk behaviors he or she has engaged in, both currently and in the past. Think about getting tested together.
It is important to take steps to reduce your risk of getting HIV. Not having (abstaining from) sex is the most effective way to avoid HIV. If you choose to be sexually active, having sex with one person who only has sex with you and who is uninfected is also effective. If you are not sure that both you and your partner are HIV negative, use a latex condom to help protect both you and your partner from HIV and other STDs. Studies have shown that latex condoms are very effective, though not 100%, in preventing HIV transmission when used correctly and consistently. If either partner is allergic to latex, plastic (polyurethane) condoms for either the male or female can be used.
What if I test positive for HIV?
If you test positive for HIV, the sooner you take steps to protect your health, the better. Early medical treatment and a healthy lifestyle can help you stay well. Prompt medical care may delay the onset of AIDS and prevent some life-threatening conditions. There are a number of important steps you can take immediately to protect your health:
- See a licensed health care provider, even if you do not feel sick. Try to find a health care provider who has experience treating HIV. There are now many medications to treat HIV infection and help you maintain your health. It is never too early to start thinking about treatment possibilities.
- Have a TB (tuberculosis) test. You may be infected with TB and not know it. Undetected TB can cause serious illness, but it can be successfully treated if caught early.
- Smoking cigarettes, drinking too much alcohol, or using illegal drugs (such as methamphetamines) can weaken your immune system. There are programs available that can help you stop or reduce your use of these substances.
- Get screened for other sexually transmitted diseases (STDs). Undetected STDs can cause serious health problems. It is also important to practice safe-sex behaviors so you can avoid getting STDs.
There is much you can do to stay healthy. Learn all that you can about maintaining good health.
Not having (abstaining from) sex is the most effective way to avoid transmitting HIV to others. If you choose to have sex, use a latex condom to help protect your partner from HIV and other STDs. Studies have shown that latex condoms are very effective, though not 100%, in preventing HIV transmission when used correctly and consistently. If either partner is allergic to latex, plastic (polyurethane) condoms for either the male or female can be used.
Why does CDC recommend HIV screening for all pregnant women?
HIV testing during pregnancy is important because antiviral therapy can improve the mother’s health and greatly lower the chance that an HIV-infected pregnant woman will pass HIV to her infant before, during, or after birth. The treatment is most effective for babies when started as early as possible during pregnancy. However, there are still great health benefits to beginning treatment even during labor or shortly after the baby is born.
CDC recommends HIV screening for all pregnant women because risk-based testing (when the health care provider offers an HIV test based on the provider’s assessment of the pregnant woman’s risk) misses many women who are infected with HIV. CDC does recommend providing information on HIV (either orally or by pamphlet) and, for women with risk factors, referrals to prevention counseling.
HIV testing provides an opportunity for infected women to find out that they are infected and to gain access to medical treatment that may help improve their own health. It also allows them to make informed choices that can prevent transmission to their infant. For some uninfected women with risks for HIV, the prenatal care period could be an ideal opportunity for HIV prevention and subsequent behavior change to reduce risk for acquiring HIV infection.







0 comments:
Post a Comment